INTRODUCTION
The Achilles tendon is the largest tendon of the body, it takes much of the load when we are running, jumping, or even walking. Achilles tendinopathy is thought to affect 150,000 people every year in the UK and accounts for 55%-65% of injuries of the achilles. This is predominatly due to overuse/over loading of the tendon. It has increased in prevelance, mainly due to increased sporting activity and intensified training. It is very common in runners, especially middle-aged, middle-distance, and long-distance runners.
The estimated prevalence in dancers is 9%, in gymnasts 5%, in tennis players 2%, and in football players less than 1%.
Insertional issues such as retrocalcaneal bursitis account for 25%-35% of cases (his pain spreads from the
The remaining diagnosed as partial tears or undiagnosed complete ruptures
Achilles Rupture
around 4500 people in the UK seek medical help for this injury each year. Individuals suffering from achilles rupture has a mean age of 37–43.5 years. It most commonly occurs when individuals are playing sport.
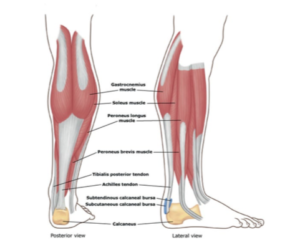
ANATOMY OF THE ACHILLES TENDON
The Achilles tendon is a common tendon shared between the gastrocnemuis and soleus muscles of the posterior leg. It connects the two muscle groups (collectively, triceps surae) to the calcaneaus. Generally, the tendon winds 90 degrees on its path towards the heel, such that the gastrocnemius attaches laterally and the soleus attaches medially. It is the thickest tendon in the human body and has the capacity to withstand large tensile forces- assisting with force transmission and acts like a spring when you push off the floor.
A subcutaneous calcaneal bursa permits movement of the skin over the flexed tendon. A deep bursa of the Achilles tendon reduces friction to allow free movement of the tendon over the bone.
Anatomy of the achilles tendon
Current thinking on treating and rehabilitation of achilles tendinopathy
Achilles tendinopathy is a common overuse injury caused by repetitive energy storage and releases with excessive compression. This can lead to a sudden injury, or in the worst case, can cause a rupture of the Achilles tendon. In both cases, a lack of flexibility or a stiff Achilles tendon can increase the risk of these injuries
The current term that is recommended to describe this pain is ‘tendinopathy’. Cook and Purdum ( 2009) proposed a new strategy when approaching tendon pain, and this is called the Tendon Continuum. The continuum model proposed a model for staging tendinopathy based on the changes and distribution of disorganization within the tendon. Three stages are as follows:
- Reactive tendinopathy-A reactive tendon is the 1st stage on the tendon continuum and is a non-inflammatory proliferative response in the cell matrix. This is as a result of compressive or tensile overload. The cells change shape and have more cytoplasmic organelles for increased protein production (proteogycans and collagen). During this process, the collagen integrity is usually maintained although some elongation separation has been shown previously. This phase is a relatively short term adaptation. This process thickens the tendon to reduce stress and increases the stiffness. On imaging the tendon does appear to be thickened and swollen due to the changes in the proteogycans. This can occur after sudden increased stress or direct impact to the tendon. At this stage the tendon has the potential to revert back to the normal tendon
- Tendon dysrepair- The progression of the reactive tendinopathy can occur if the tendon is not offloaded and allowed to regress back to the normal state. During this phase, there is the continuation of increased protein production which has been shown to result in separation of the collagen and disorganisation within the cell matrix. This is the attempt of tendon healing as with the 1st phase but with greater involvement and breakdown physiologically. This is now visible on MRI and ultrasound scans. Also, there may be evidence of increased vascularity and neural ingrowth within the tendon. This phase has been said to be a difficult one to diagnose so history taking is essential, the most accurate method to diagnose this stage is through imaging. This phase of tendinopathy can be developed by frequently overloading the tendon in phase 1 of the continuum. This phase can be developed much more quickly in the older stiffer tendon as there is less flexibility and adaptivity readily available in the tissues
- Degenerative tendinopathy-This is the final stage on the continuum and is suggested that at this stage there is a poor prognosis for the tendon and changes are now irreversible. It has been documented that there areas of cell death, trauma and tenocyte exhaustion and general disorganisation of the cell matrix. On imaging, there are areas of this degeneration scattered throughout the tendon and interspersed with normal sections of tendon and parts of the tendon that are in the dysrepair phase. The tendon can be thickened and present with nodular sections on palpations. Clinically this tendon is present in the older individual who has had ongoing problems with tendinopathy, or the younger individual who has continued to overload the tendon
It has been suggested that the tendon can move up and down this continuum and this can be achieved through adding or removing load to the tendon especially in the early stages of tendinopathy and this is how we rehabilitate our clients that we see presenting with tendinopathy.
The Movement Perfected Team are trained to assess and treat AChilles INJURIES
The major goals of general rehabilitation of the Achilles are:
- Gain full ROM of the ankle ( knee to wall to test for Dorsi flexion and test passive plantar flexion to rule out posterior impingement), inversion and eversion
- Repair muscle strength and proprioception
- Gain good functional stability
- Reach the best possible functional level (walking, running, jumping…)
- Decrease the risk for re-injury
- Return to sport/previous level of activity and or beyond
Return to sport testing
Before you return to your sport we at Movement Perfected would test the injured ankle and progress it through three stages of rehabilitation to ensure it has the strength and stability to return to sport as safely as possible.
These exercises include:
Supine calf isometric with band
Stage 1 exercise: These isometric contractions are performed to about 70% of your maximum contraction, they are held for 45 seconds, and are repeated for 5 rounds with a 2-minute rest break in between.
single leg heel raise
Isotonic exercises such as the single leg heel raise are great in addition to eccentric exercises for numerous reasons when optimizing how to rehab achilles tendinopathy. Isotonics will additionally strengthen the muscle, treat the mind-muscle connection, strengthen the kinetic chain, and address the compression loads needed for high-level activities.
.
SINGLE WALL HOPS
Hands on to the wall and hopping repeatedly up and down, to ensure the leg is comfortable with repetative plyometric loads.
We would test the above and a battery of tests releative to your sport or movement goal To give the all clear and confidence that you are ready for action.